Metro Colon Rectum - Proctology Corner – Pilonidal Disease
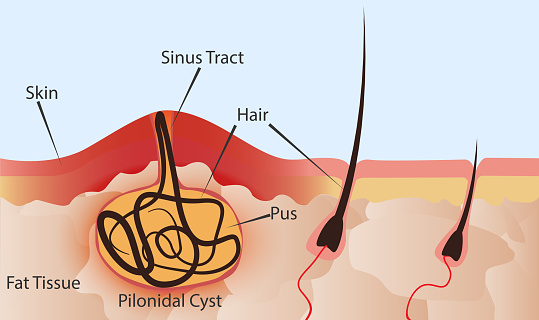
Pilonidal disease is caused by trapped hair and debris in the pores of the natal cleft (the area above your butt cheeks). Through dynamic motion the pores of the natal cleft open and close collecting foreign material. This material festers and can form a sinus tract. If the sinus tract becomes infected, an abscess forms. Sometimes the abscesses drain spontaneously but most require surgical drainage for symptom relief. Pilonidal disease occurs in less than 0.1% of the population with a slight male predominance. The risk factors for pilonidal disease are a deep natal cleft, prolonged sitting, increased hair density or local trauma / irritation.
Pain with fevers and drainage are the usual presenting symptoms to the proctologist’s office and if the area is acutely infected, treatment can usually be rendered in the office. While symptoms might improve with office-based therapy, definitive surgery is usually required to eradicate the sinus tract. Antibiotics alone are insufficient to treat the sinus or abscess because the antibiotics do not destroy the sinus tract and cannot penetrate the abscess cavity.
There are many surgical techniques described for the treatment of pilonidal disease. These range from pit picking, incision and drainage, excision with marsupialization or excision with flap closure. Marsupialization is when the wound is left open and the walls of the wound are sewn into the base of the wound. This provides a wide based wound that is easy to pack and has a higher chance of closing from the bottom up. A flap is healthy tissue from another (local) area of the body that is moved into the wound. Flaps are usually saved for repeat disease or large defects. The key tenet in all these procedures is to destroy the sinus and prevent its re-occurrence through the regrowth of healthy tissue in the natal cleft.
My preference is to primarily address pilonidal sinus’ through incision or excision with marsupialization if needed. I find that this provides excellent destruction of the sinus and allows for slow wound healing in the natal cleft. These wounds can take months to heal but are less likely to reoccur because the wound heals without creating a potential space. When primary surgical attempts fail I pivot to flap based repairs as the secondary surgical excisions are traditionally more extensive and moving healthy tissue into the secondary surgical site can help increase rate of healing. I do not like flaps for the primary surgery because if the flap fails, not only does the pilonidal sinus typically reoccur but the tissue used for a flap typically cannot be used again.
Post operatively, the patient can expect a chronic wound that will need daily dressing changes with gauze and tape. Showers and baths are ok and I encourage patients to scrub the pilonidal wound (if they did not have a flap) to help encourage the body to heal. The patient can expect bleeding from the wound for one to two weeks following the procedure. The bleeding is controlled with gauze and pressure.
While pilonidal sinuses and abscesses can be frustrating, surgical options are approachable and efficacious. Know that you are not alone and that your neighborhood proctologist is happy to help.