The Colon and Rectum
• Colon
Ascending, Transverse, Descending, Sigmoid
Primary purpose is water reabsorption
• Rectum
Final 14-20cm of the large intestine
Primary purpose is stool repositor
Colon and Rectal Cancer - Epidemiology
• One of the top five causes of cancer
• 4% lifetime chance
• Declining by 2.5% per year over the last two decades
• Earlier diagnosis through colonoscopy saves lives
• Curable
• Start from a polyp
Polyps
• Can develop in all parts of the colon and rectum
• Start as non-cancerous growths from the inner lining (mucosa)
• Grow and evolve over 3-8 years from adenoma to adenocarcinoma
• Most do NOT become cancer (hyperplastic / inflammatory polyps)
Polyps – Risk Factors for Cancer
• Most form for unknown reasons – 75%
• Family History – 18%
• Rare genetic conditions– FAP (APC), HNPCC (MMR) – 6%
• Familial and sporadic
• Inflammatory conditions – Inflammatory bowel disease – 1%
Colon and Rectal Cancer – Symptom
• Unexplained weight loss
• Blood in stool
• Change in bowel function or narrow stools
• Vague abdominal pain without a diagnosis
• Colonoscopy is the gold standard for diagnosis
Colonoscopy Basics
• Starts at age 45 or 10 years before earliest family member diagnosis
• Outpatient procedure, One day off work
• Bowel preparation starts the night before after 5:00pm
• Painless, twilight sedation
• A small camera that traverses the large bowel from the anus to the end of the small intestine
• Can remove pre-cancerous polyps and reduce lifetime risk
Colonoscopy Biopsy and Polypectomy
• Adenocarcinoma
• Other forms
Squamous
Carcinoid
GIST
Lymphoma
Staging Colon and Rectal Cancer – Imaging
• Computed Tomography Scan
Chest / Abdomen / Pelvis
• Magnetic Resonance Imaging Scan
Pelvis / Liver
• Positron Emision Tomography Scan
Staging Colon and Rectal Cancer - TNM
• T Score – Involvement of the colon wall
Penetrating mucosa (1), submucosa (2), muscularis (3), serosa (4)
• T Score – Involvement of the rectal wall
Penetrating mucosa (1), submucosa (2), muscularis (3), mesorectal fat (4)
• N Score – Involvement of the regional lymph nodes
1-3, 4+
• M Score – Involvement of distant sites
Present or absent
Staging Colon and Rectal Cancer - TNM
• Stage 1 – Local Disease – surgery can cure
T1, T2 – N0
• Stage 2 – Local Disease – surgery can cure
T3, T4 – N0
• Stage 3 – Nodal Disease – chemotherapy is needed
N1,N2
• Stage 4 – Metastatic Disease – chemotherapy is needed
M1
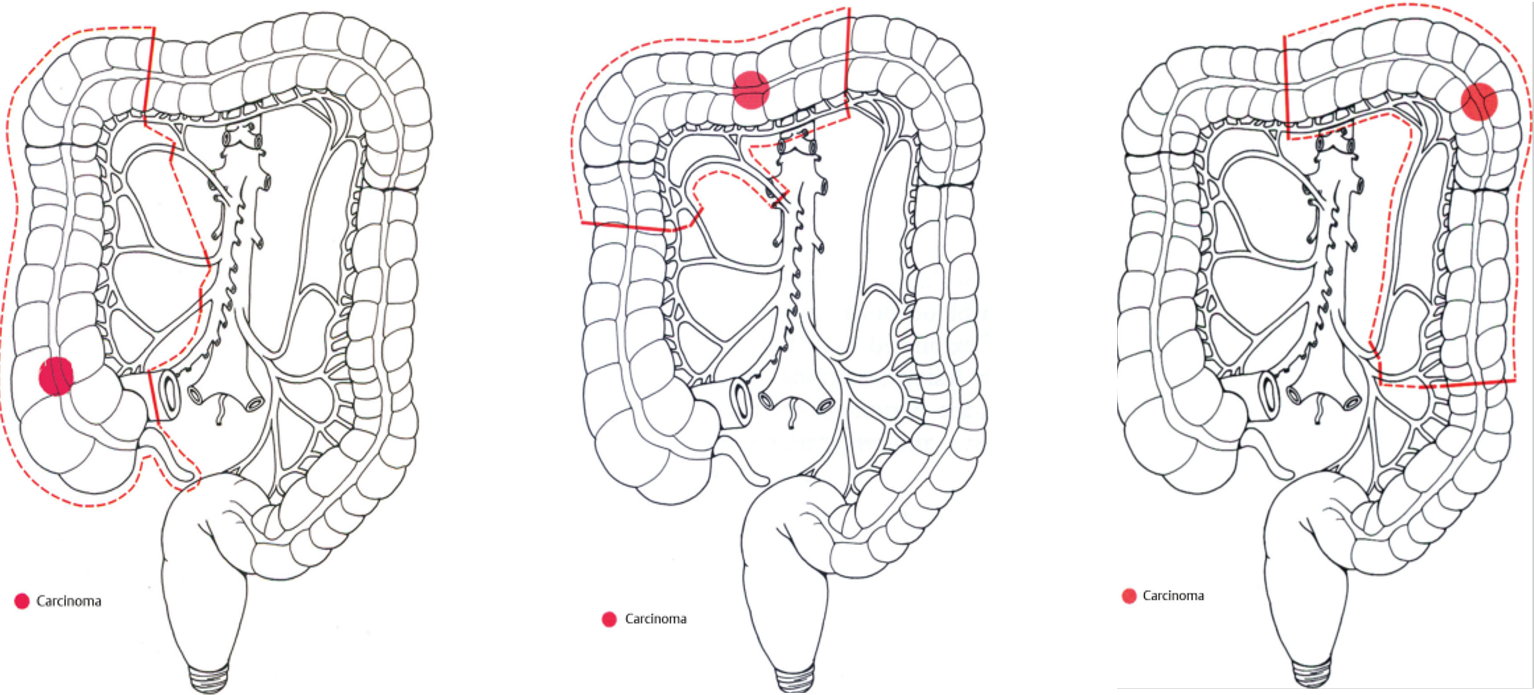
Colon Cancer Treatment
• Surgical excision is beneficial for stage 1,2,3 and sometimes 4
• Chemotherapy can be administered following surgery
Some new data to suggest immunotherapy can help pre surgery
• Radiation is not utilized unless fixed margins are present
• Ostomy utilization is less common
Rectal Cancer Treatment
• Surgical excision is beneficial for stage 1,2,3 and sometimes 4
• Chemotherapy and radiation are best administered prior to surgery
Six months of treatments constitute total neoadjuvant treatment (TNT)
Better patient tolerance
Better oncologic outcomes
• Ostomy utilization is more common
General Tenets of Surgical Treatment
• Identify and restore normal anatomy
• Mobilize colon or rectum
• Establish tumor free margins
Proximal/distal
Radial, en bloc
• Ligate feeding vessel for lymph node sampling
• Re-establish continuity of GI tract (if possible)
Colon Cancer - Anastomosis
Rectal Cancer – Distance to Sphincter is Key
• The distal margin is crucial for continence preservation
5cm is the old surgical dogma
2cm is the new surgical dogma and removes microscopic disease
1cm is acceptable if it preserves continence and TNT was completed
Rectal Cancer – APR
Colon and Rectal Cancer - Pathologic Staging
• Derived from the surgical specimen
• Like clinical staging but based on histologic assessment by a clinically specialized pathologist
True stage
Can change from pre-operative stage
• T/N/M
• Margin status
• Genetic features
Colon and Rectal Cancer - Surveillance
• Clinical
• Serologic
• Radiographic
• Endoscopic
Colon and Rectal Cancer - Survivorship
• Physical
Change in bowel function, nerve damage, ostomy management
• Emotional
Change in lifestyle, stigma, sexual dysfunction
• Financial
• Treatment, transportation, lifestyle changes, disability
Healthy habits
Cancer screening
General health care
Diet and exercise – goal of 150 minutes per week
Alcohol reduction, smoking cessation
Colon and Rectal Cancer – Conclusion
• Colon and Rectal cancer are both curable when detected early
• Colonoscopy and cancer screening tests are accessible
• Establish a support structure at home and with your care team