Metro Colon Rectum - Proctology Corner – Rectal Prolapse
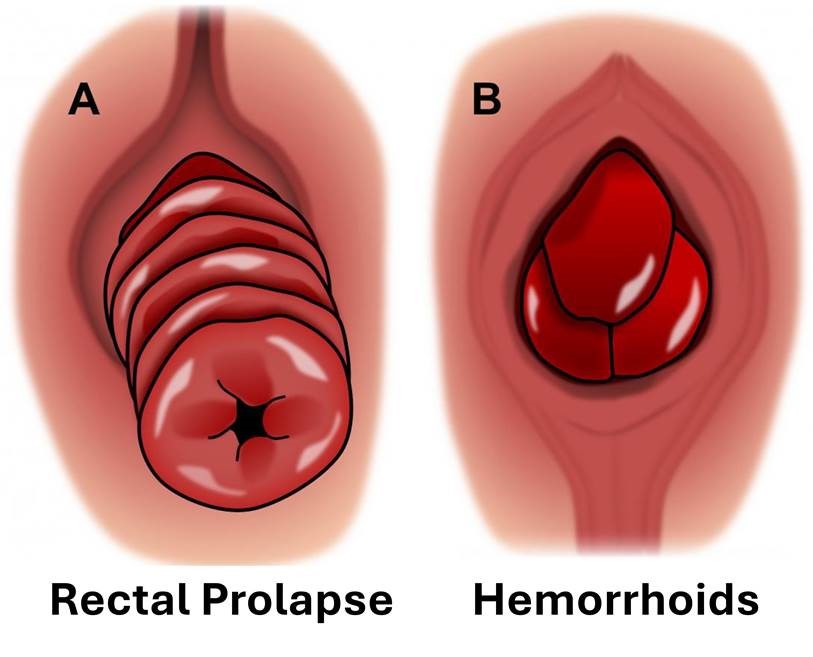
Rectal prolapse is a full thickness protrusion of the rectum through the anal canal. This is different from hemorrhoidal prolapse which is the contents of the anal canal protruding externally. Colloquially, rectal prolapse looks like “a cinnamon bun” while hemorrhoid prolapse usually looks like “three knuckles”. Both rectal prolapse and hemorrhoids can present with mucus discharge, bulging, bleeding, constipation, leakage, anal spasm and pelvic pain. Both rectal prolapse and hemorrhoids are primarily due to increased abdominal pressure. Statistically, women are six times more likely to develop rectal prolapse; this problem usually starts in their 70s.
The work up for rectal prolapse starts in the proctologist’s office with a detailed history and physical exam including proctoscopy. This helps confirm the extent of rectal prolapse and identify causative factors like constipation or straining as well as identify prolapse of other organs or urinary symptoms which can impact the treatment offered. A colonoscopy is usually offered to help rule out a lead point for the prolapse in the colon or rectum. Once the diagnosis is confirmed the patient is risk stratified.
Surgical options for rectal prolapse are grouped into abdominal or perineal procedures. Perineal procedures, Delorme and Altmeier, involve removing redundant rectum from below. This procedure does not enter the abdomen and can be indicated for patients with prior abdominal surgery or patients who would not tolerate general anesthesia. The recurrence rate for perineal rectal prolapse procedures can reach 40%. Mesh is not generally used in these procedures.
Abdominal procedures, suture rectopexy and rectosigmoidectomy, enter the abdomen and reduce the redundant colon and rectum and suspend the redundant segment to the sacrum (the tailbone). For the rectosigmoidectomy a segment of redundant colon is removed from the body and a stapled connection is made to reconnect the colon to the rectum. The bowel is not divided or entered for the suture rectopexy and no connection is required. General anesthesia is required for an abdominal procedure. The recurrence rate for an abdominal procedure is less than 5%. Mesh is not generally used in these procedures for the first prolapse.
The suture rectopexy is our preferred rectal prolapse repair because of its low recurrence rate. The suture rectopexy is performed robotically through five small incisions. Patients are generally discharged from the hospital the morning after surgery with very little discomfort. Following surgery bowel function will evolve over six to eight weeks as the anal muscles adapt. Recurrence of prolapse is possible especially if the underlying cause is not also addressed. Surgery for recurrent prolapse is more complicated and usually has a higher rate of subsequent recurrence.
Rectal prolapse symptoms can be lifestyle limiting and surgical options are effective. Robotic rectopexy is the preferred procedure given its safety profile, its efficacy and its fast recovery.
The source of the image: https://fascrs.org/patients/diseases-and-conditions/a-z/rectal-prolapse-expanded-version