Metro Colon Rectum - Proctology Corner – Obstructed Defecation
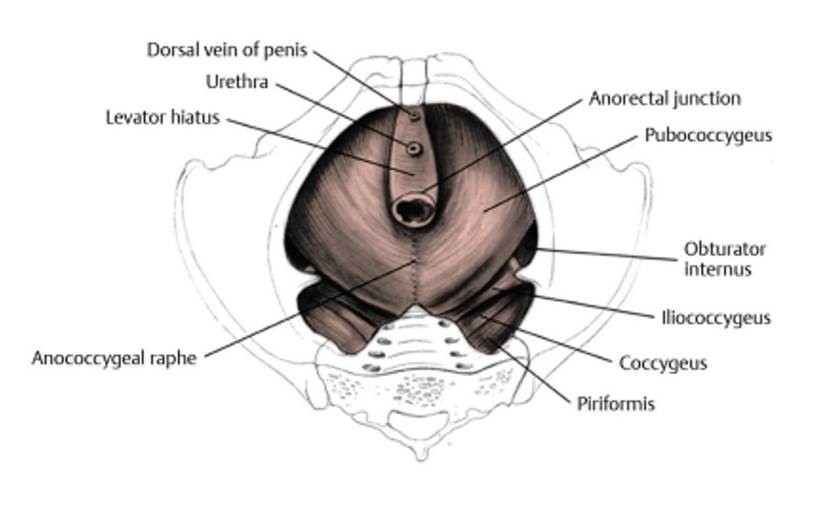
Obstructed defecation is the group of diagnoses relating to constipation caused by confusion of the pelvic floor muscles or ineffective evacuation secondary to mechanical changes in the pelvis. Obstructed defecation is sometimes called: levator spasm, non-relaxation of the puborectalis, anismus, rectocele, enterocele, or internal intussusception. Obstructed defecation is characterized by excess straining, incomplete evacuation, external manipulation to defecate or requiring numerous cathartics to defecate. Obstructed defecation can sometimes be confused for fecal incontinence or rectal prolapse given the medications and maneuvers patients adopt to defecate. Obstructed defecation is treatable and rarely requires surgery involving physical therapy and pelvic retraining to establish an improved quality of life.
The diagnosis of obstructed defecation starts with a comprehensive office-based history and physical exam including proctoscopy. The office exam helps uncover any medical, physical, psychological issues that may contribute to obstructed defecation. Prior surgery, prior trauma and life stress can all contribute to derailing the complex interactions that facilitate defecation. Based on the preliminary findings additional studies may be ordered. If the patient has not recently undergone a colonoscopy, endoscopic clearance of the colon and rectum will be prioritized.
The three primary studies for diagnosing obstructed defecation are anal manometry, MRI defacography, and a colon transit study. Anal manometry involves an office-based examination of the anorectal area using a balloon with pressure sensors. Anal manometry will determine rectal sensitivity, sphincter strength and the anal canal ability to sample solid/liquid/gaseous material. MRI defecography is performed with radio-opaque paste and a special toilet that facilitates a cross-sectional image of the pelvis while defecation occurs. MRI defecography will identify changes in muscle contraction during defecation and identify any internal intussusception. Prolapse of the vagina/uterus, bowing of the rectum into the vagina or downward pressure from the small bowel can also be identified during MRI defecography. Colon transit studies use special markers (sitz marker) to track how quickly food moves through the gastrointestinal tract. Colon transit studies require confirmation with X-ray studies.
Interpretation of the results will allow for a tailored treatment regimen. All treatment regimens stsart with good hydration and fiber supplementation. Including 1-2 liters of water daily with 30-40g of fiber and modest exercise will stimulate colonic motility and increase bowel frequency. Pelvic floor physiotherapy can also be very effective in retraining the pelvic floor muscles to relax and contract at the correct phase of defecation. Sometimes psychological therapy can be effective if a causal factor was traumatic. Surgery is appropriate in rare cases of obstructed defecation.
To summarize, obstructed defecation is very frustrating for patients and can cause lifestyle limiting symptoms. A tailored diagnostic regimen is important and will involve multiple functional tests. Obstructed defecation can be effectively treated without surgery and the overall prognosis is good.
The source of the image: Beck et al., Gordon and Nivatvongs’ Principles and Practice of Surgery for the Colon, Rectum, and Anus, 4th Ed. (ISBN 978-1-62623-429-1)