Metro Colon Rectum - Proctology Corner – Fecal Incontinence
Fecal incontinence is defined as the uncontrolled passage of stool for at least three months in an individual who previously had control. Fecal incontinence can be lifestyle limiting and can co-exist with other pelvic floor disorders. In most cases, fecal incontinence is due to ineffective sphincter function and is more common as we age. Fecal incontinence can also be made worse by injury to the sphincters, injury to nerves that control the sphincters or by gastrointestinal motility disorders. Given the wide range of causes for fecal incontinence, the diagnosis and treatment is tailored to the individual.
The workup for fecal incontinence begins by understanding the extent of the loss of control and identifying contributing factors. Standardized questionnaire forms are used to quantify the frequency and severity of incontinence symptoms to help establish a baseline and track progress. An office-based examination is helpful in identifying anatomic abnormalities and is supported by objective measurements of sphincter strength and rectal sensation (anal manometry). Anal ultrasound and magnetic resonance imaging can also provide clarity of functional causes of incontinence. If a patient has not had a colonoscopy recently, it will also be recommended to rule out other nefarious pathology.
Conservative management is always considered initially and is successful in 25-50% of individuals. Conservative management consists of dietary fiber supplementation, fluid management and medication optimization. Specific attention is paid towards substances that can trigger fecal urgency like caffeine, artificial sugars, gluten and lactose. Medical treatments focus on slowing the bowels and thickening the stool. Noninvasive bowel training can also be helpful and consists of scheduled enemas or suppositories or colonic lavage. Pelvic floor rehabilitation provides the next step in conservative management and functions to strength and synchronize the sphincter complex.
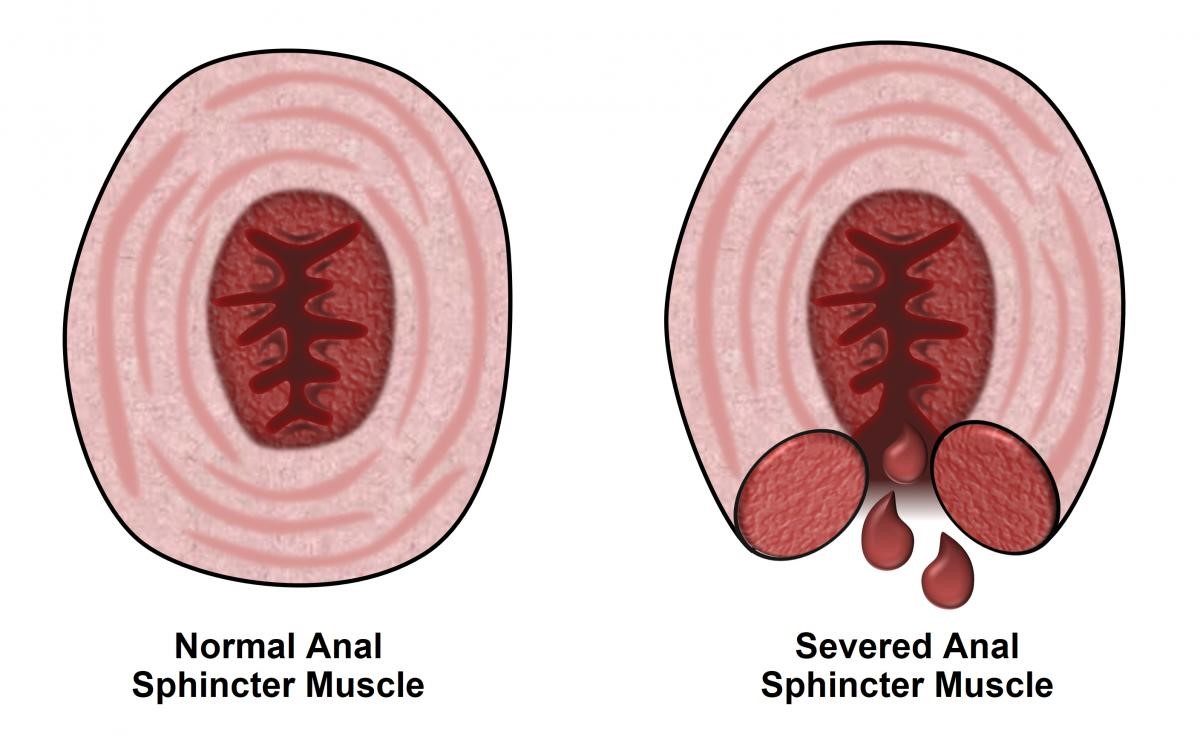
When conservative management remains unsuccessful, surgical options are entertained. Depending on the nature of the incontinence and the integrity of the sphincter complex treatment can range from recreation of the anal sphincter ring (sphincteroplasty) to implantation of a sacral nerve stimulator. Sphincteroplasty is most effective with a clinically apparent sphincter defect and shows good short term results in up to 85% of individuals. The durability of sphincteroplasty deteriorates over five years to less than 20% efficacy. Repeat sphincteroplasty is generally not performed. Sacral nerve stimulators are utilized for both fecal and urinary incontinence with promising results. These devices are FDA approved and are implanted into the nerves of the sacral spine. A generator is implanted into the buttocks in a separate surgery. The device is then controlled remotely to tailor nerve stimulation to patient symptoms and can be changed over the life of the device. Short- and long-term results are promising for individuals who experience success with sacral nerve stimulation.
We understand that fecal incontinence is a very frustrating issue to address and recognize the stigma fecal incontinence can generate. Treatments are tailored based on multiple modalities of testing to personalize each patient’s experience. Please do not hesitate to contact us with questions.
The source of the image: https://fascrs.org/patients/diseases-and-conditions/a-z/fecal-incontinence